When Your Bladder Hurts: Understanding the Basics
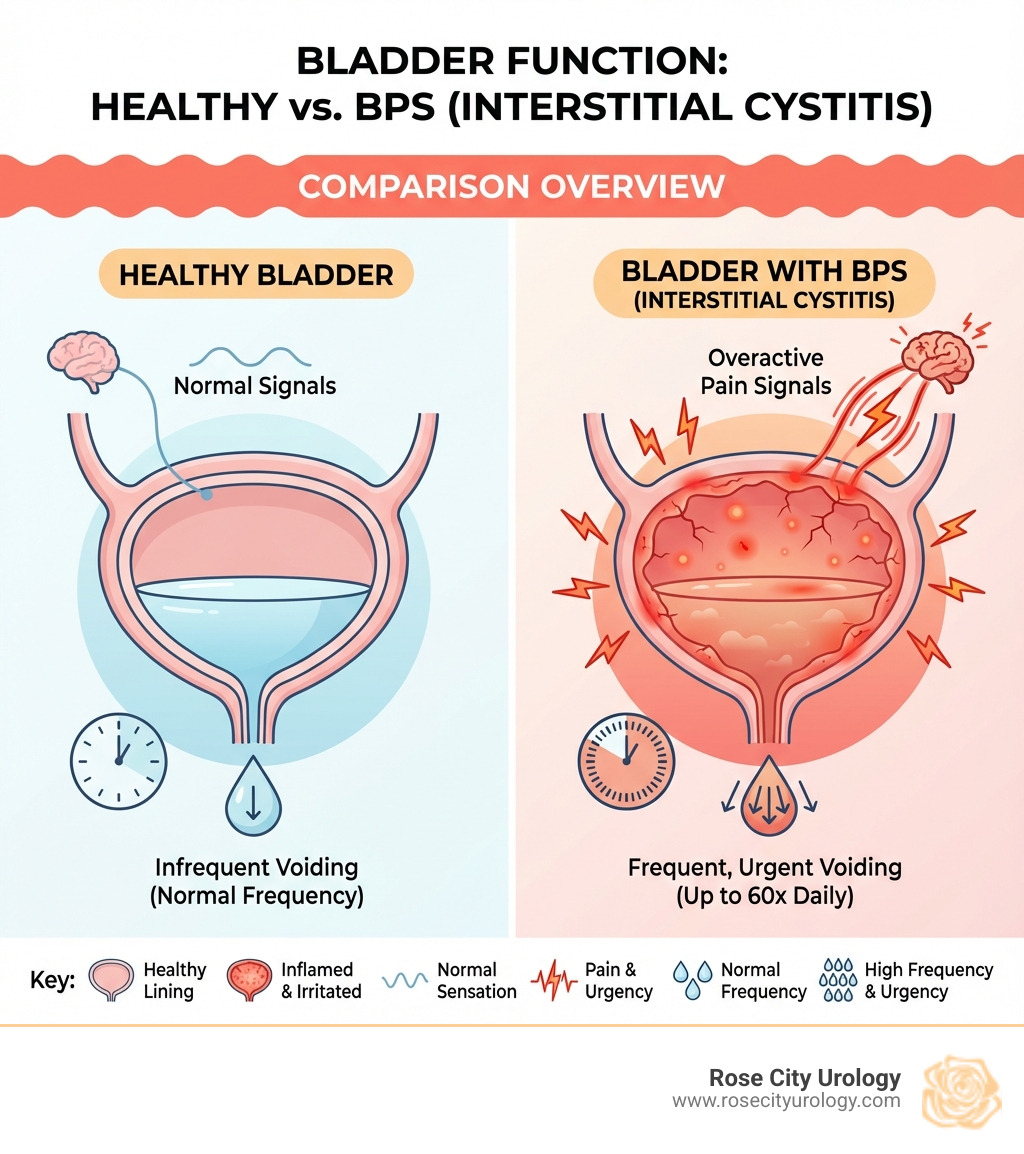
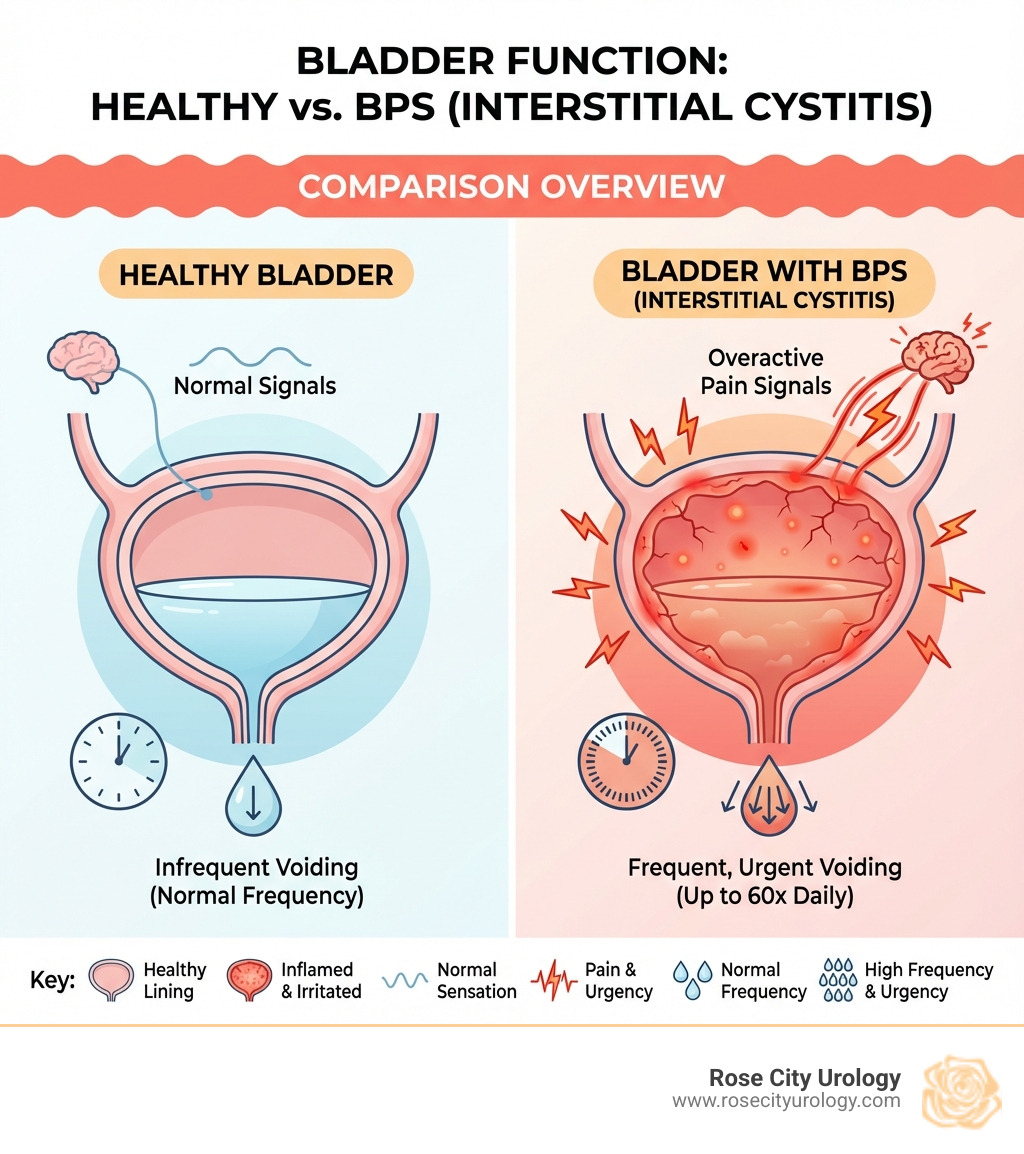
Bladder pain syndrome (BPS), also called interstitial cystitis (IC), is a chronic condition causing pain and pressure in the bladder area. It involves urinary symptoms lasting over six weeks without an infection or other clear cause.
Quick Overview: What You Need to Know
- What it is: A chronic bladder condition causing pain, pressure, and frequent urination
- Who gets it: Mostly women (2-3 times more than men), usually age 30+
- Main symptoms: Bladder/pelvic pain, urgent need to urinate, frequent urination (sometimes up to 60 times daily)
- Diagnosis: Based on symptoms lasting 6+ weeks after ruling out infections and other conditions
- Treatment: No cure, but multiple treatment options can manage symptoms effectively
- Prevalence: Affects 1-6% of people in the United States (approximately 3-8 million women and 1-4 million men)
BPS is often misdiagnosed because there's no single test to confirm it. Instead, doctors diagnose it by ruling out other conditions like urinary tract infections, overactive bladder, or bladder cancer.
The condition can significantly impact quality of life, leading to disrupted sleep, work difficulties, strained relationships, and emotional challenges like anxiety or depression.
The good news is that while BPS is chronic, most people can find relief. Personalized treatment plans combining lifestyle changes, medications, and other therapies often provide meaningful improvement, though it may take several weeks or months.
As a board-certified urologist at Rose City Urology, I'm Dr. Ryan Tubre. I've helped many patients steer Bladder Pain Syndrome using a range of treatments. My goal is to partner with you to find the right therapies to improve your symptoms and restore your quality of life.
Common Bladder pain syndrome vocab:
Understanding Symptoms, Causes, and Risk Factors
Bladder pain syndrome (BPS), or interstitial cystitis (IC), is a complex chronic condition affecting the bladder. Our team at Rose City Urology understands the challenges this condition presents and is here to help you steer its complexities.
Common Signs and Symptoms
The hallmark of BPS is bladder-related pain, pressure, or discomfort, which can be constant or intermittent. These symptoms mimic a urinary tract infection (UTI) but occur without any infection.
Common signs include:
- Pain with Bladder Filling: Pain that worsens as the bladder fills and is temporarily relieved by urination. It's typically felt above the pubic bone but can also occur in the perineal area.
- Frequent Urination: A persistent need to urinate far more often than average—sometimes up to 60 times a day—including at night (nocturia).
- Urgency: An intense, compelling need to urinate that often doesn't respond to standard overactive bladder (OAB) therapies.
- Pain During Sexual Intercourse (Dyspareunia): Women often experience pain during or after sex. Men may have pain after orgasm or in the genital/rectal area, with over 70% reporting sexual dysfunction.
- Symptom Flares: Symptoms vary and can fluctuate, with periods of sudden worsening ("flares") that last for hours, days, or weeks. Common triggers include menstruation, stress, exercise, and sexual activity.
If you have chronic bladder symptoms lasting more than six weeks without a clear cause, we encourage you to contact us at Rose City Urology.
What Causes Bladder Pain Syndrome?
The exact cause of BPS is unknown, but several theories exist.
- Bladder Lining (Urothelium) Defect: A defect in the bladder's protective GAG layer may allow substances in urine to irritate the bladder wall, causing inflammation and pain.
- Inflammation and Mast Cell Activation: Chronic inflammation involving mast cells, which release histamine and other inflammatory chemicals, may contribute to pain and urgency.
- Autoimmune Response: The body's immune system may mistakenly attack the bladder. This is supported by the link between BPS and other autoimmune diseases like lupus and rheumatoid arthritis.
- Neurogenic Inflammation and Nerve Changes: Bladder nerves may become hypersensitive, sending false or amplified pain signals to the brain and creating a constant sense of fullness.
- Associated Conditions: BPS often coexists with other chronic pain disorders, such as:
- Irritable Bowel Syndrome (IBS)
- Fibromyalgia
- Chronic fatigue syndrome
- Endometriosis
It's likely a combination of these factors contributes to BPS. Our focus at Rose City Urology is on effectively managing your symptoms.
Who is at Risk?
Certain factors increase the risk of developing BPS:
- Gender: Women are diagnosed two to three times more often than men.
- Age: Most people are diagnosed in their 30s or older.
- Family History: A family history of BPS may increase your risk.
- Other Chronic Pain Syndromes: Having conditions like fibromyalgia or IBS increases the risk.
- Autoimmune Diseases: A link exists with autoimmune conditions like lupus and Sjögren's syndrome.
- Men and Misdiagnosis: Men with BPS are often misdiagnosed with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). BPS should be considered if standard prostatitis treatments fail. You can read more about scientific research on IC risk factors here: Scientific research on IC risk factors.
At Rose City Urology in Tyler, TX, we are attuned to these risk factors and ensure a thorough evaluation for all our patients.
How Bladder Pain Syndrome is Diagnosed
Diagnosing Bladder pain syndrome is a process of elimination, as there is no single definitive test. At Rose City Urology, our comprehensive evaluation aims to identify your condition accurately while ruling out other possibilities.
The diagnostic journey begins with:
- Symptom Duration: Symptoms must have lasted for at least six weeks.
- Ruling Out Infection: A urinalysis and urine culture are done to rule out a urinary tract infection (UTI).
- Medical History: We conduct a detailed discussion about your symptoms, their duration, severity, and potential triggers.
- Physical Examination: This includes a general physical, a pelvic exam for women, and a neurological exam to check for pelvic floor muscle tenderness and other conditions.
- Bladder Diary: You may be asked to keep a voiding log to track fluid intake and urination frequency.
- Urine Tests: Besides checking for infection, urine cytology may be used to rule out bladder cancer, especially for smokers.
Diagnostic Tests and Procedures
While diagnosis relies heavily on symptoms, certain tests can provide valuable information:
- Cystoscopy: This procedure uses a thin camera (cystoscope) to look inside the bladder and rule out other conditions like cancer or strictures. During the procedure, we look for:
- Hunner's Ulcers (Lesions): Red, inflamed patches on the bladder wall found in 5-10% of BPS cases. Their presence is diagnostic for classic IC.
- Glomerulations: Small, pinpoint bleeding spots that can appear after the bladder is stretched. They are common in BPS but not specific to it.
- Biopsy: A small tissue sample may be taken during cystoscopy to help rule out other conditions.
- Urodynamic Testing: These tests measure bladder function. While not diagnostic for BPS, they can help identify other issues. A small bladder capacity is a common finding.
- Potassium Sensitivity Test (PST): This test checks if a potassium solution causes pain, suggesting a damaged bladder lining. It is not universally recommended.
Comparing Bladder Symptoms: BPS vs. Other Conditions
This table highlights why a thorough diagnostic process is essential:
| Symptom | Bladder Pain Syndrome (BPS) | Urinary Tract Infection (UTI) | Overactive Bladder (OAB) |
|---|
| Pain | Chronic bladder/pelvic pain, often worse with filling, relieved by emptying | Burning during urination, general discomfort, lower abdominal pain | Usually no pain, but may have discomfort from urgency |
| Urgency | Persistent, intense urge to urinate, even after emptying | Sudden, strong urge to urinate | Sudden, strong urge to urinate |
| Frequency | Frequent urination (often small amounts), day and night (nocturia) | Frequent urination | Frequent urination, day and night (nocturia) |
| Urine Test | Negative for infection | Positive for bacteria/white blood cells | Negative for infection |
| Duration | Chronic (>6 weeks) | Acute (days to weeks), resolves with antibiotics | Chronic |
| Other Symptoms | Can have associated pain during sex, IBS, fibromyalgia | Fever, chills, nausea (if kidney infection), cloudy urine | May have urge incontinence |
An accurate diagnosis is key to creating an appropriate treatment plan for your Bladder pain syndrome.
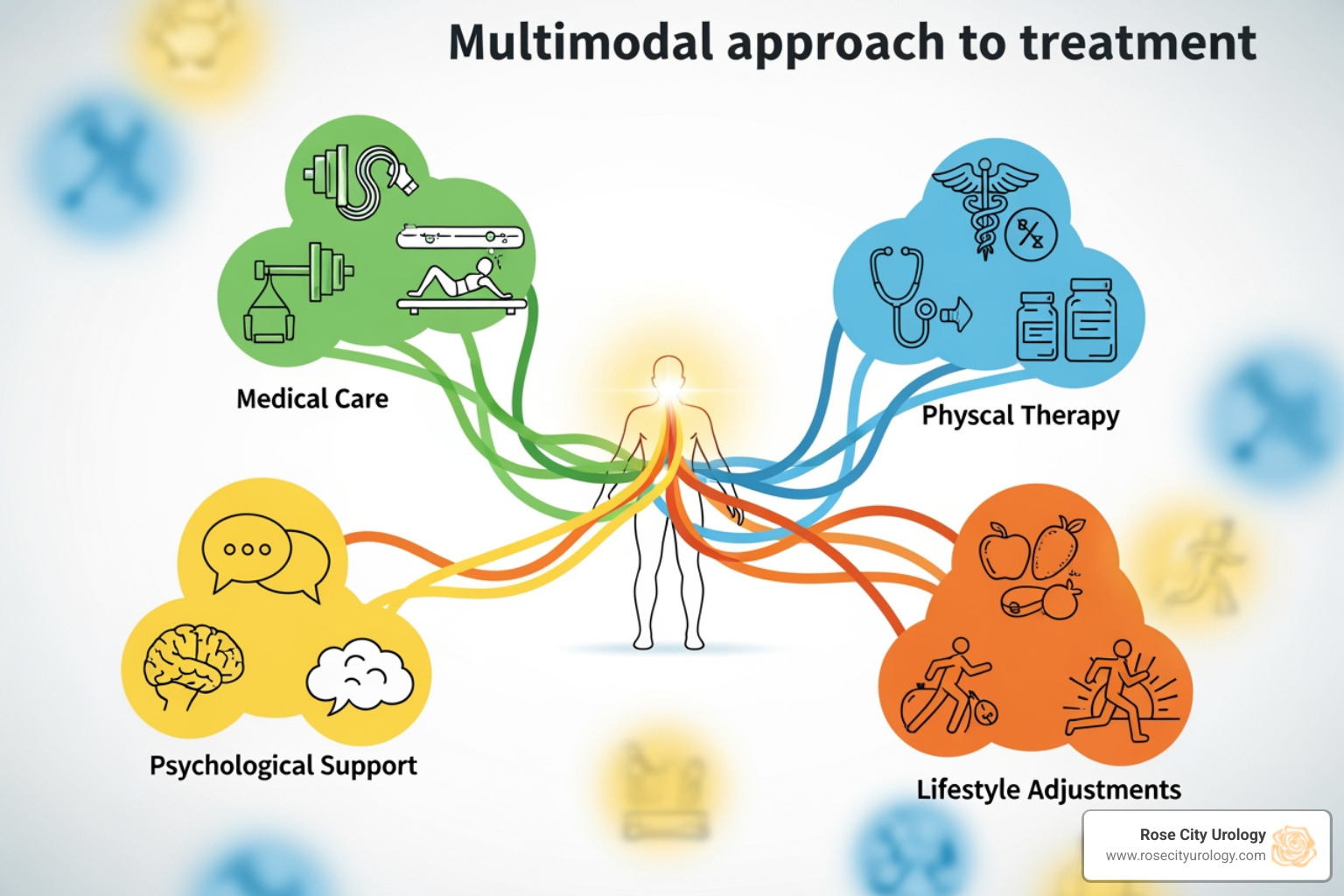
Comprehensive Treatment for Bladder Pain Syndrome
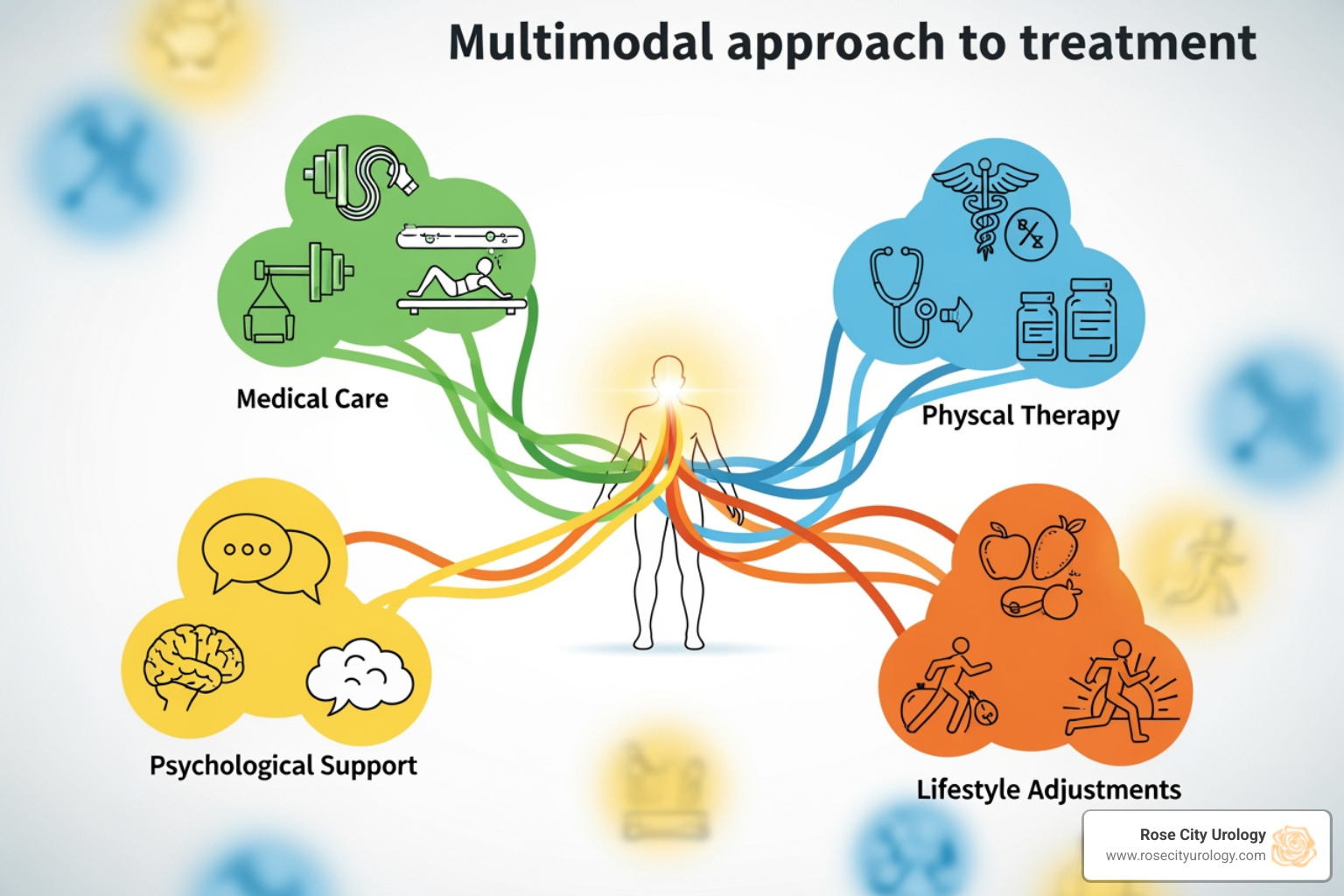
There is no one-size-fits-all solution for Bladder pain syndrome. At Rose City Urology, we create a personalized, multimodal treatment plan that combines different approaches to control your symptoms. Finding relief can be a journey, but we are committed to working with you every step of the way. It may take weeks or months to see improvement.
Lifestyle and Dietary Management
Lifestyle and dietary changes are often the first step in managing BPS and can significantly reduce symptom flares.
- Elimination Diet: We often recommend an elimination diet to identify your specific food and drink triggers. This involves avoiding common irritants, then reintroducing them one by one. Common triggers include caffeine, alcohol, tomatoes, spicy foods, artificial sweeteners, and carbonated drinks.
- Stress Reduction: Stress can worsen BPS symptoms. Techniques like mindfulness, meditation, and gentle yoga can be very helpful.
- Gentle Exercise: Low-impact exercises like walking or swimming can help, but avoid activities that increase your pain.
- Bladder Retraining: This behavioral therapy helps increase the time between urination to improve bladder capacity and reduce urgency.
- Other Self-Care: Wearing loose clothing, using heat or cold packs, and avoiding prolonged sitting can also provide relief.
The Role of Physical Therapy
Pelvic floor physical therapy is a crucial second-line treatment, especially for patients with pelvic floor muscle tenderness.
- Myofascial Release: Manual therapy techniques can release tension and trigger points in the pelvic floor muscles, significantly reducing pain.
- Relaxation Exercises: The focus is on relaxing and lengthening pelvic floor muscles, not strengthening them.
- Avoiding Kegel Exercises: Standard strengthening exercises like Kegels can worsen BPS symptoms and are generally not recommended.
We can guide you to appropriate physical therapy resources in the Tyler, TX area. For more information, visit our page on More info about bladder control services.
Medications for Symptom Relief
When other measures aren't enough, medications can help manage symptoms.
Oral Medications:
- Amitriptyline: A tricyclic antidepressant used to reduce pain, frequency, and urgency.
- Hydroxyzine: An antihistamine that can reduce urgency and frequency.
- Pentosan Polysulfate Sodium (Elmiron): The only FDA-approved oral drug for BPS. It may help repair the bladder lining but can take 3-6 months to work and requires monitoring for a serious eye condition.
- Cyclosporine A: An immune-suppressant for severe, refractory cases.
- Gabapentin: An anti-seizure drug that can help reduce neuropathic pain.
Bladder Instillations (Intravesical Therapy):
These medications are delivered directly into the bladder via a catheter.
- Dimethyl Sulfoxide (DMSO): Reduces inflammation and blocks pain signals.
- Heparin: Believed to help repair the damaged GAG layer.
- Lidocaine: A local anesthetic that provides temporary pain and urgency relief.
- Hyaluronic Acid and Chondroitin Sulfate: Thought to help restore the bladder's protective barrier.
- Triamcinolone: A steroid used to reduce inflammation, especially with Hunner ulcers.
Procedures and Surgical Options
For patients who don't find relief with other treatments, we offer several advanced options.
- Cystoscopy with Hydrodistension: Stretching the bladder with water under anesthesia can provide temporary relief from pain and frequency.
- Fulguration of Hunner's Ulcers: Cauterizing these ulcers during cystoscopy often provides significant relief.
- Nerve Stimulation (Neuromodulation): Mild electrical impulses are sent to nerves controlling the bladder.
- Sacral Neuromodulation: Implanted devices like Axonics Therapy stimulate the sacral nerves to improve bladder control and reduce pain.
- Percutaneous Tibial Nerve Stimulation (PTNS): A less invasive option that stimulates a nerve in the ankle to affect bladder function.
- Botulinum Toxin (Botox) Injections: Injected into the bladder muscle to reduce spasms, pain, and urgency. Patients must be willing to self-catheterize if urinary retention occurs. Learn more on our Bladder Botox page.
- Major Surgery (Cystectomy): A last resort for severe, intractable cases, this involves bladder removal and is rarely performed.
Living with Bladder Pain Syndrome
Living with Bladder pain syndrome requires resilience and a strong support system. While it's a chronic condition, our goal at Rose City Urology is to help you manage your symptoms effectively so you can lead a fulfilling life.
Impact on Daily Life and Long-Term Outlook
BPS can significantly affect physical, emotional, and social well-being.
- Sleep Disruption: Waking at night to urinate (nocturia) is common and leads to chronic fatigue.
- Social and Work Challenges: The constant need for restroom access can make social outings difficult and interfere with work productivity.
- Emotional Distress: Living with chronic pain often leads to anxiety, depression, and frustration.
- Sexual Intimacy: Pain during sex is common for women, and men report high rates of sexual dysfunction, which can strain relationships.
Long-term Outlook:While BPS is chronic, the outlook for symptom management is positive.
- Chronic but Manageable: Symptoms can be managed effectively with a personalized treatment plan.
- Remission and Flares: Many people experience periods of remission followed by flares.
- Improved Quality of Life: With appropriate, multidisciplinary care, most individuals can achieve significant improvements in their symptoms and quality of life.
Finding Support and Resources
Navigating life with BPS is easier with the right information and support.
- Support Groups: Connecting with others who share your experience can be validating and helpful for sharing coping strategies.
- Patient Advocacy Organizations: Organizations like the Interstitial Cystitis Association (ICA) provide invaluable education, advocacy, and community.
- CDC Research Efforts: The CDC is actively researching BPS to better understand its causes, links to other conditions, and long-term effects, and to address health disparities in diagnosis and treatment. You can learn more about What the CDC is doing to address IC/BPS.
Our team in Tyler, TX, is dedicated to providing comprehensive care that supports both your physical and emotional well-being.
Conclusion
Bladder pain syndrome is a challenging chronic condition, but it is manageable. While there is no cure, our goal at Rose City Urology is to create a personalized, multimodal treatment plan to significantly improve your symptoms and quality of life. We combine lifestyle changes, physical therapy, medications, and advanced procedures to help you find relief.
Our team in Tyler, TX, offers expert urologic care in a supportive environment. Don't let Bladder pain syndrome control your life. There is hope for improvement, and we are here to guide you on your journey to better bladder health.
Contact us to discuss your bladder health concerns.